Can you call it a tonsillectomy update when no tonsillectomy took place? Well, there is much to report.
1) Tonsils -Apparently her tonsils are now so small that he wouldn't remove them. He says he has only been in this situation a handful of times. The good: no painful recovery. The bad: there will be no improvement in her swallow or airway since there was no surgery done.
2) Adenoids- They were fairly large so he went ahead and did a partial removal (not full, since that tends to cause nasal speech in kids with low muscle tone.)
3) Her soft palate and uvula are very close to the wall of her throat. This is not good and worries him that she would develop sleep apnea if she were decannulated (during the day it's less of a problem). Our options: We could remove part of the soft palate and uvula. Yes, that's done. And no they don't put the uvula back after they reduce the soft palate. Apparently we don't really need the uvula and doctors in East Africa remove it routinely. Still that doesn't sound so great to me. Of course we could also try CPAP if it turned out that she needed it post-decann but my guess is he doesn't expect that to be successful. I wonder if this could have been caused by her craniofacial reconstructions because the advancement of the forehead causes the mid face growth to halt or slow. I don't recall them ever mentioning it being "too close" before. I will ask the ENT at our next appointment if a mid-face advancement (which Ainsley may need at some point in the future to reallign her jaw and bring the middle of her face back forward) would do the same thing.
4) Tongue- Her tongue sits kind of far back in her throat. It isn't clear if it causes an obstruction, although it is possible that it contributes to the problems. But there isn't much that can be done for that if it turns out to be the case.
4) Tongue- Her tongue sits kind of far back in her throat. It isn't clear if it causes an obstruction, although it is possible that it contributes to the problems. But there isn't much that can be done for that if it turns out to be the case.
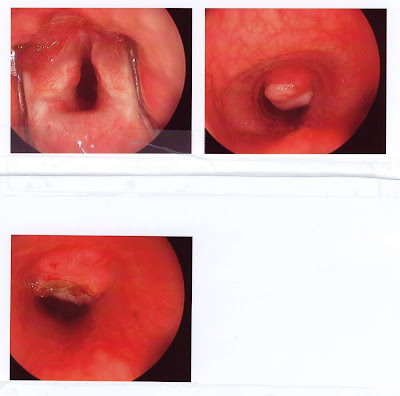
5) Granuloma - I knew she had a granuloma. In the past I think they didn't remove it, thinking there was no need, and that it would likely grow back. But this time he decided to remove it. Pictures are below. He is actually hoping that this improves her airway since this mass is no longer obstructing airflow. Of course it could grow back. They often do. This is a common side effect of having a trach.
Are you tired yet? I am, but WAIT there's MORE.
6)Collapse of the trachea - She has a fair degree of collapse on the wall of her trachea from the hole where the trach is. This is another common side effect of having a trach. He doesn't think it is severe enough to cause a big problem in itself but we aren't necessarily out of the woods completely for needing a laryngotracheosplasty(LTP).
8) Scarring- the terrible scarring and fixation of her vocal cords and arytenoids didn't look so back to him this time. So that's good. Really good. It explains why I've been hearing more varied vocalizations from her. The bad news is that it meant he couldn't laser anything to help her out. Or maybe that's good.
9) Ear Tubes- He did note an unusual cresent shape with a ridge on the front part of both eardrums. What this is/means who knows but he didn't think it should cause any loss of function. He didn't note any changes to the eardrums that would indicate a need for tubes and since tubes can cause problems he opted not to place them. That's fine with me, even though this past year she's been hit with a lot of ear infections. I'll hope that it improves on it's own.
9) Ear Tubes- He did note an unusual cresent shape with a ridge on the front part of both eardrums. What this is/means who knows but he didn't think it should cause any loss of function. He didn't note any changes to the eardrums that would indicate a need for tubes and since tubes can cause problems he opted not to place them. That's fine with me, even though this past year she's been hit with a lot of ear infections. I'll hope that it improves on it's own.
10) Capping- He says she SHOULD be able to cap. That kids have to get used to it. But wait, didn't he also say she might need a cricoid split to open the glottic area??? I guess this means we are back to trying to cap. Probably unsuccessfully.
I don't know about you, but my head was spinning after all this. WTH does all this mean? .....The road to decannulation could be tricky with lots of potholes on the way. There are plenty of things that could go wrong. Is any of that a surprise to me? No. Where does this leave us? We will watch her closely over the next weeks hoping that the granulation removal opened up her airway quite a bit and that she has an easier time capping. Then he wants to see her for a scope while she's awake in the office in the next month or two to see what is going on while she is breathing. Then I guess we might start talking surgical options.
Upper Left: Vocal cords. Much more open than in the past. Upper Right: The granuloma Lower Left: The granuloma area after removal.
Ainsley has been happily napping since we got home before noon. I expect her to recover fairly easily, especially since the tonsils didn't come out, but we have good pain meds just in case. There will be associated swelling with the procedures so I don't think we'll know how much it will help her for at least a week maybe more but be sure I will let you know as soon as I do.



.JPG)







I'm glad she doesn't have any recovery issues, but sad that they were not able to 'help" with any of the issue they went in for. I hope the granuloma removal gets some good results...and likewise the capping. So is the thought that she would cap during the day & use the Trach only at night due to the possibility of obstructive apnea?
ReplyDeleteYou always work up to capping at night. We have never tried night capping because day capping has been a bit of a struggle(her airway wasn't really adequate). He's trying to think through the big picture and eliminate the chance of a failed decann. When (read IF) she can make it through the days capped we'll move to capping at night, but he may require a sleep study first.
ReplyDelete